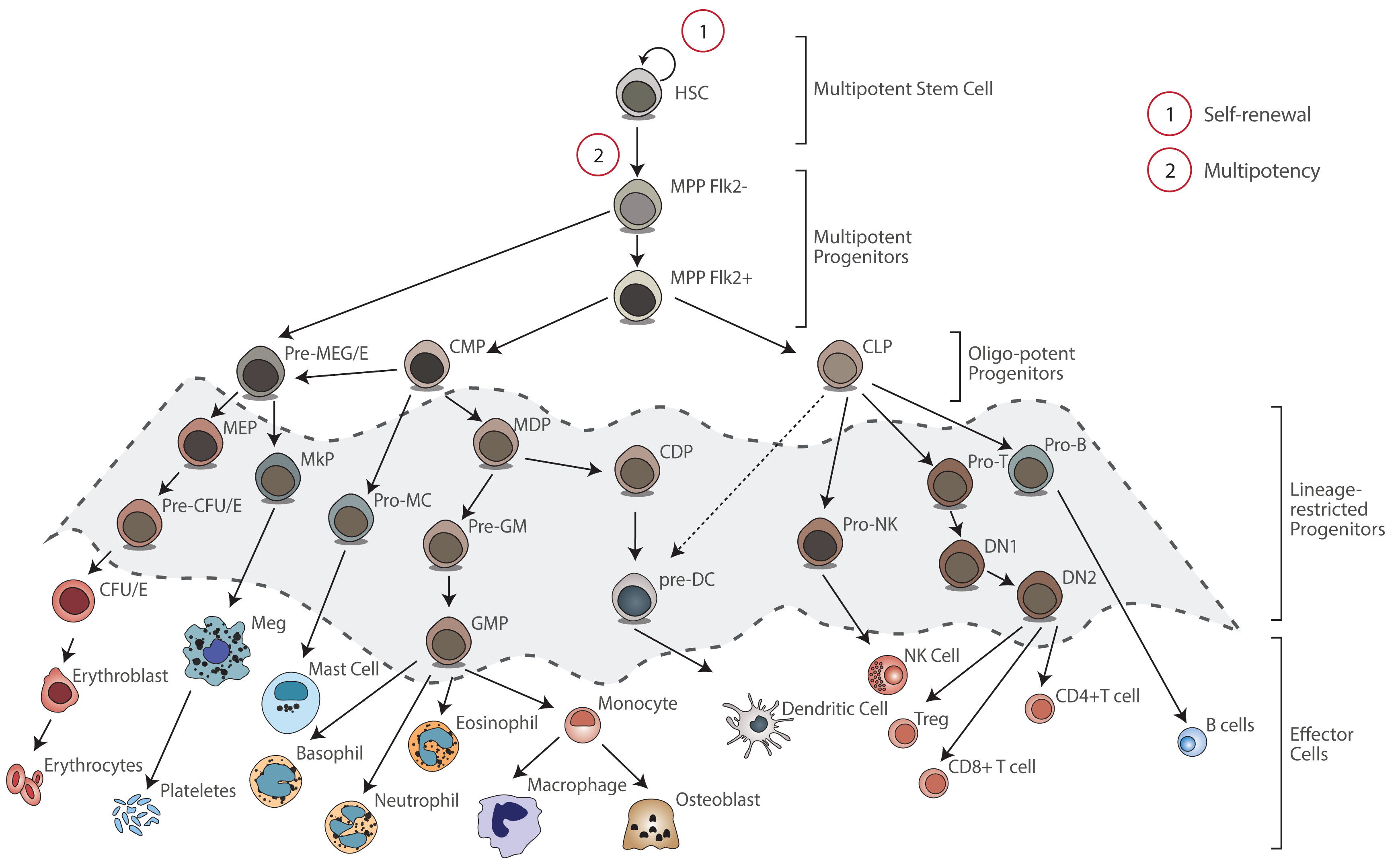
Blood cells are generated by the proliferation and differentiation of a very rare population of multipotent stem cells named hematopoietic stem cells (HSCs). HSCs are defined by a combination of 2 core properties:
1. Self-renewal: allows HSCs to maintain the stem cell program after cell division.
2. Multipotency: HSCs have the capacity to generate any differentiated blood cell.
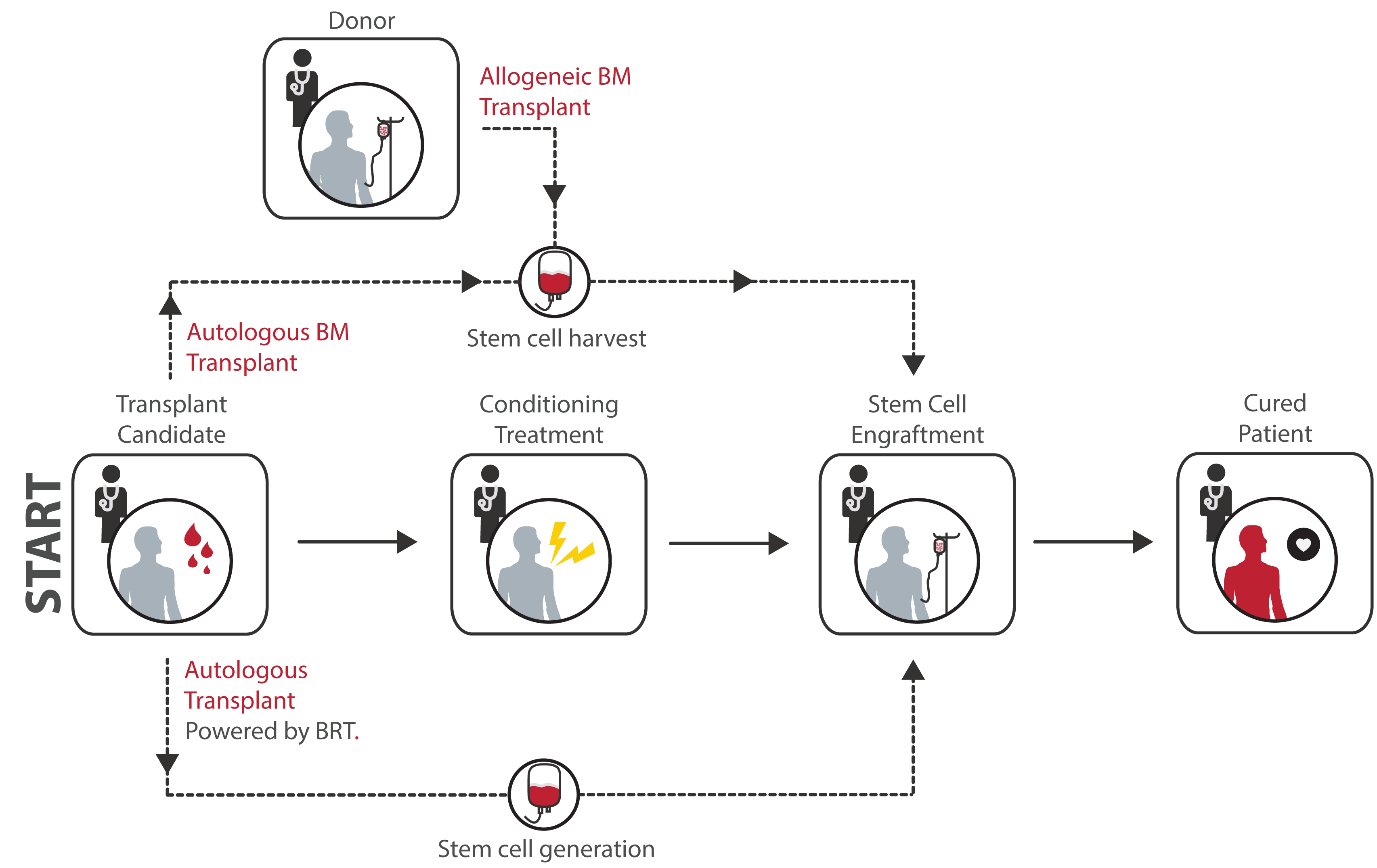
Since the rst HSC transplant in 1957, stem cell transplantation has been used to treat over 1 million patients worldwide. In fact, for some of the most devastating disorders a ecting the blood-forming process, stem cell transplantation is the only potential curative treatment. Transplantation of HSCs involves the intravenous infusion of autologous or allogeneic HSCs collected from bone marrow (BM), peripheral blood, or umbilical cord blood to reestablish hematopoietic function in patients with damaged or defective BM or immune system. In addition, HSC transplant is used to allow patients with cancer to receive higher doses of chemotherapy than BM can usually tolerate. BM function is then reestablished by replacing the BM with autologous or allogeneic HSCs.
When a patient is eligible for a stem cell transplant, the patient's (autologous) or donor`s (allogeneic) stem cells are typically harvested from peripheral blood via apheresis. Before transplant, the patient receives conditioning treatment consisting in high doses of chemotherapy with or without radiation. This treatment is able to destroy patient's stem cells, opening space in the bone marrow for the new transplanted stem cells. After transplant, the new cells are able to engraft in the bone marrow and to regenerate the blood system. We will provide an alternative source of autologous HSCs for transplantation purposes.
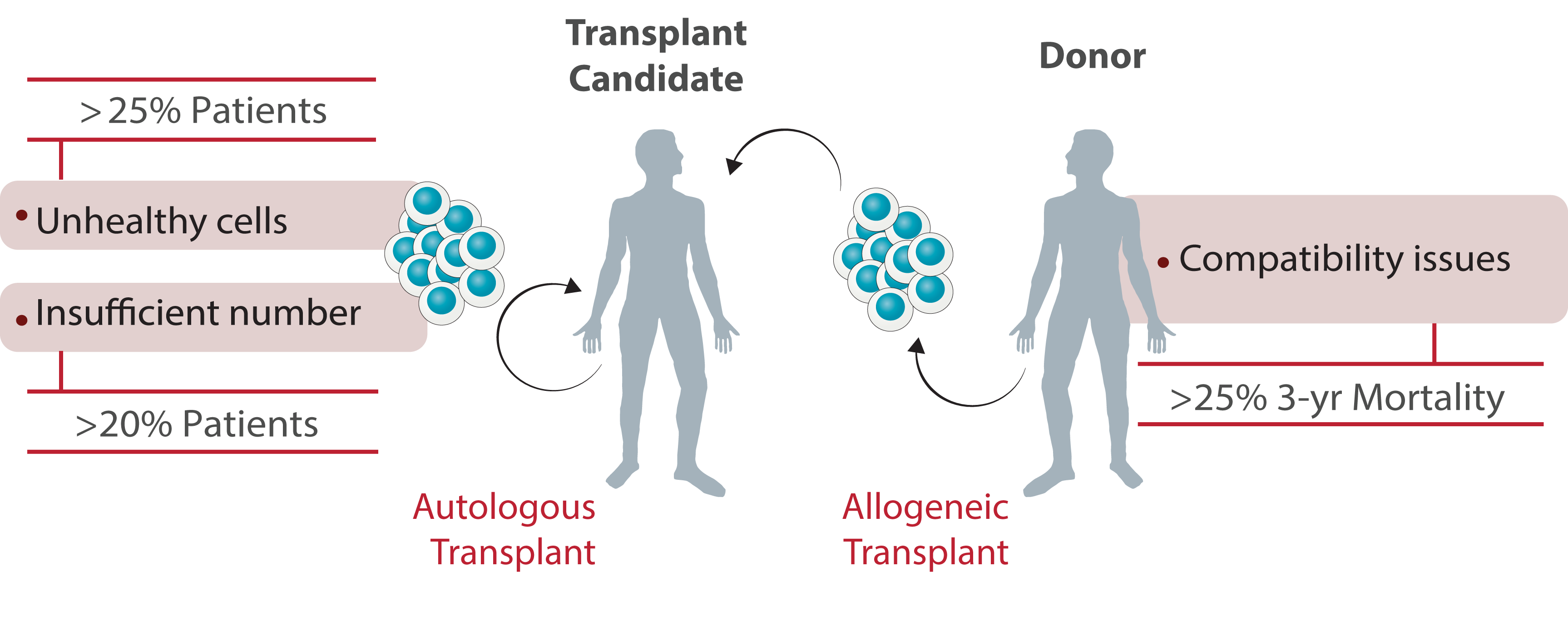
Despite the increasing demand for HSC transplant in the past decades and the constant clinical improvements, stem cell transplantation is still considered a high-risk procedure associated with several complications with intensive and costly medical care requirements. The lack of healthy and compatible HSCs, provided in su cient number for transplantation, justify these complications and the use of this procedure as a last-resort therapy only for patients with life-threatening disorders.